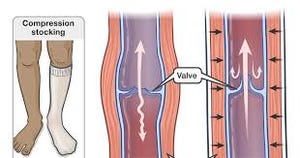
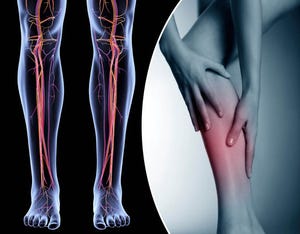
Compression Socks and How They Help with Lymphedema
For individuals experiencing lymphedema, compression socks represent a valuable tool in their treatment arsenal. By effectively managing swelling, improving circulation, and alleviating pain, compression socks can significantly enhance the quality of life for those affected by this condition.